|
|
What is Peroneal (Ankle) TendonitisWhen You Roll Your Ankle and the Pain is on the Outside of the Foot, You Have Most Likely Strained the Peroneal Tendons Peroneal Tendonitis is the Most Common Form of Ankle Tendonitis, and Has a Pain Pattern Along the External Side of the Ankle.You might be suffering from Peroneal Tendinitis if you have:
Peroneal Tendon - Location & Function
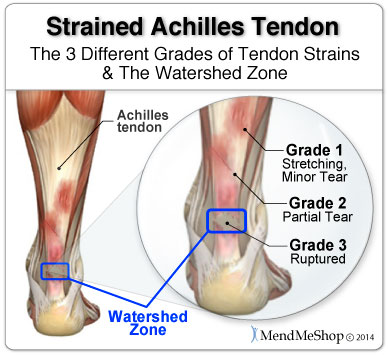
There are a number of tendons (fibrous tissue that connect muscle to bone) in the foot which help to control movement while you are walking or running. Two ankle tendons commonly injured are the peroneus longus and the peroneus brevis, and together, these are known as the peroneal tendons. These 2 long tendons have acquired this name because they harness most, if not all, the strength pertaining to the outside of the leg/ankle. The peroneal tendons are important tendons because they prevent the foot from rolling and causing a lateral (inversion) ankle sprain. The superior peroneal retinaculum and inferior peroneal retinaculum ligaments run over top of the 2 peroneus tendons holding them close to the calcaneus (heel bone). If these 2 tendons were cut, you would have no ability to prevent your foot from turning inward when you walk, effectively causing constant ankle rolling. If these tendons are overstrained and too long, you will find the same thing happening - you will be frequently having ankle inversion sprains. Peroneal tendons are long, attaching to outer leg muscles then running behind and underneath the bone (fibula) on the outside of the ankle. For some people, injury can cause the natural holding structure to fail and allow these tendons to slip over the bone. In such cases, this is usually called a peroneal tendon dislocation. When they slip into this position the peroneal tendons become slightly weaker than the muscles and tendons on the inside of the ankle. Due to this (you probably guessed it), you are more likely to roll your ankle inward and sprain it on a frequent basis. The "Peroneal Tendon" is actually a name give to two tendons: the Peroneus Longus and the Peroneus Brevis. Together, they are harness all the strength pertaining to the outside of the ankle (this is known as "lateral ankle strength") Peroneal Tendonitis, Peroneal Tears, and TenosynovitisPeroneal Tendon Dislocation (subluxation) or Tearing may occur in one or both of these tendons. This leads to pain, swelling, sensitivity and a sense of instability behind the outside of the ankle. They can also pop out of the supporting ligaments that hold them in place which is called a dislocation. Once this occurs, continuous or recurrent dislocation and tearing may occur without immediate attention and repair. Stitching and at the worst, tendon replacement may be required for patients suffering from torn or dislocated peroneal tendon(s). 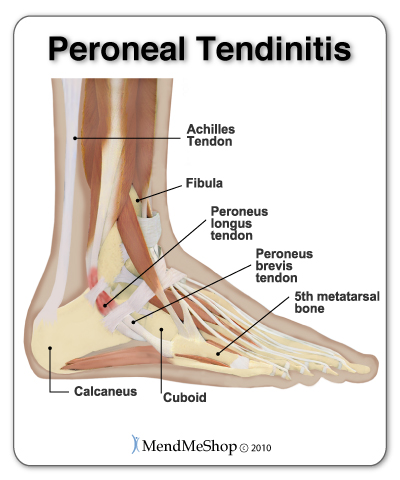 Peroneal tendonitis (also spelled tendinitis) is the inflammation and irritation of one or both of the peroneal tendons. Like all forms of tendonitis, peroneal tendonitis is a condition that may flare up and subside over a period of time. Peroneal tendinitis is usually caused by repetitive use of the tendons, but can also be caused by trauma such as a rolled or sprained ankle. Little tears in the peroneus longus tendon and the peroneus brevis tendon irritate the tendon fibers resulting in pain and inflammation. Peroneal tenosynovitis is swelling and inflammation of the peroneal tendons' sheaths (or coverings) which prevents the tendons from gliding smoothly within the sheaths causing pain. It can be experienced at the same time of peroneal tendonitis, and has similar symptoms. It often results in trouble moving the ankle and will feel sore to the touch. In rare cases, tenosynovitis can be caused by infection, so it is always recommended to check with your doctor to rule this out as a cause. Tearing of the peroneus longus tendon and/or the peroneus brevis tendon can occur. This leads to pain, swelling, sensitivity and a sense of instability in the ankle. The tendon(s) can also pop out of the supporting ligaments that hold them in place (superior peroneal retinaculum and inferior peroneal retinaculum ligaments) which is known as dislocation. Who is Most at Risk of a Peroneal Tendon Injury?
Symptoms of Peroneal Tendonitis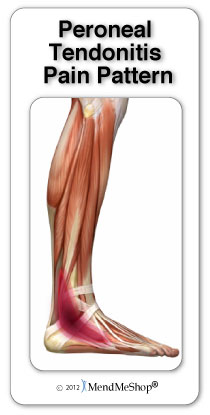 Peroneal tendon injuries may happen suddenly through an acute incident / accident / trauma or develop over a period of time from over-use or re-injury (a chronic condition). If you have peroneal tendonitis you may feel:
It is important to recognize pain in these areas compared to pain over the fibula (your ankle bone) which might indicate a different problem like a stress reaction of the bone or fracture. Pain on the fibula occurs directly over the bone which is easily felt with your fingers. Peroneal tendon injuries are sometimes misdiagnosed and may worsen without proper treatment, prompt opinion by a foot and ankle doctor is advised. Peroneal Tendonitis DiagnosisThe diagnosis of peroneal tendonitis is usually made by examination of the ankle. A physical check by your doctor will help to determine where the tendons are inflamed, ruptured, or degenerated. The doctor will move your ankle into different positions during a physical examination. The peroneal tendons are checked by holding your foot up and out against the doctor's downward pressure. Stretching the foot up and in can also be used to test whether the tendons hurt. The doctor will also be looking for instability of your ankle joint, swelling, warmth and weakness on the outer side of your ankle. X-rays may be ordered to make sure there is no fracture or other problem with your fibula or the other bones in your ankle. Your doctor may order a magnetic resonance imaging (MRI) scan of your ankle. These images can show if there is abnormal swelling or scar tissue in the tendons. MRI scans can also show lengthwise tears in the tendons. Causes of Peroneal TendonitisPeroneal tendonitis is the degeneration of the tendon tissue in the ankle. What causes our tendon to start to fall apart? 
What You Need to Successfully Treat Your Peroneal Tendinitis Injury:
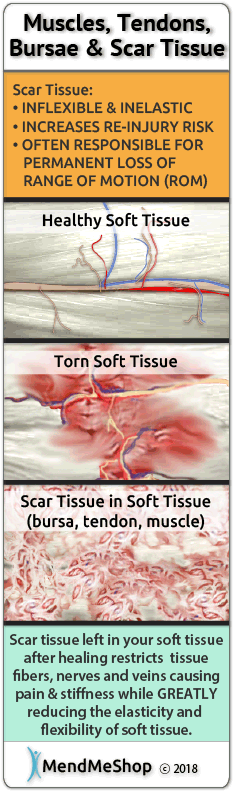
These 2 tools are what you need for rapid healing. These are the tools that top professional athletes use to treat their injuries every day. And just like these athletes, you can treat yourself at home. In fact, if you want to heal properly you have to treat yourself because you need to treat your injury every single day. If you have a Peroneal Tendon Injury, it's important to heal it quickly and completely. If you don't, it may plague you on and off again for years and cause more debilitating injuries due to over-compensation. Nonsurgical Treatment for Peroneal TendonitisIf you have a lot of pain you may need to have a walking boot or cast for 2 to 4 weeks. If there is no pain or tenderness with walking a stirrup ankle brace, arch support, or lateral heel wedge can help to take tension off of your injured tendons. In most cases, your Doctor will start with non-surgical treatments options. Some of the options your doctor may recommend include drugs or medications like NSAIDs (non-steroidal anti-inflammatory drugs) to manage pain and inflammation. Steroid injections are advised with caution for any type of tendon condition as there is increased risk of tendon rupture. Restricted Movement Is Risky If It Goes On For Too Long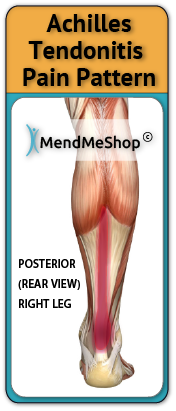 For acute (new or recent) Achilles tendon tears that have the ability to heal on their own - your doctor may even cast your foot in a toe pointed position (in something called a "hanging enquinus cast") or in a removable brace/splint. A removable splint can be very helpful to prepare you for PT sessions and mobility exercises. Prolonged use of a cast, removable splint, or long-term rest (restricted movement) without proper exercise or stretching can make your Achilles tendon injury worse. If your Achilles tendon remains completely immobilized and at constant rest, the ends of the Achilles tendon (where it attaches to bone or other muscles) will begin to fill in with scar tissue as part of the healing process. You may also have on-going symptoms of pain, swelling and inflammation, and even poor blood flow circulation. Lack of proper blood flow and growth of scar tissue will decrease the natural length of the tendon (atrophy) and tighten tissue, reducing the flexibility between your ankle and foot. Your ability to push off with your foot in certain activities such as running, jumping, or going up and down stairs all become compromised. You are also at an increased risk of re-rupture of the tendon, especially if the initial injury was large and required surgery in the first place. Peroneal Tendon Injury Scar Tissue Growth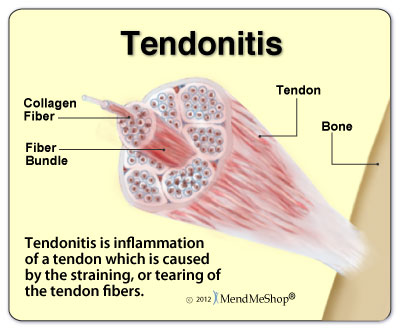 The tendon tries to protect itself from this constant irritation by trying to repair the damaged tissue. During the healing process your body will automatically fill in tears in your tendons with dense, brittle tissue called "scar tissue". The human body will use scar tissue as a temporary healing solution and will try to build the scar tissue as fast as possible to heal tears in your peroneal tendons. Scar tissue can form fast to strengthen the damaged tendon, but working fast doesn't mean that the job's done right. When scar tissue forms it doesn't come together as neatly as regular (healthy) tendon tissue would. Scar tissue fibers will lay down over top of your tear in a cluttered, messy and jumbled up way. 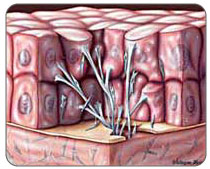 This is how scar tissue works. The scar tissue that forms in and around your strained ankle tendons will be unorganized and won't line up properly with the healthy tissue surrounding the tear. This scar tissue will also attach to everything in and around your ankle including the surrounding healthy tissue as well. This can result in a long-term fusing together of your tendon with everything around it; this will definitely freeze up your ankle, severely reducing your mobility. Scar tissue is a weak form of collagen - hard, inflexible, and tough to get rid of once it begins to take hold. The more scar tissue that develops, the more you lose range of motion. With excess scar tissue build up, the injured soft tissue and the ankle in general will remain weak and prone to re-straining and re-tearing. While you can go a number of days and even a few weeks without any major setbacks during the injury.. inevitably, a certain movement or motion will happen that causes your injured soft tissue to strain and even tear once again. This is attributed to the scar tissue build up and will result in the buildup of yet more scar tissue and a further reduced range of motion (ROM). The more scar tissue that develops, the greater the risk of winding up permanently injured with chronic pain or arthritis. Scar tissue means that your joint will not perform as well as it once did and it makes it much more prone to injury later on. The longer the injury remains, the risk of atrophy increases and the risk of more scar tissue increases. This is why it is critical to treat your tendon injury now rather than later. Continuous re-injury and build-up of scar tissue makes it more likely that you will wind up with chronic pain, reduced Range of Motion or even arthritis (permanent damage).Nonsurgical Treatment for Peroneal TendonitisIf you have a lot of pain you may need to have a walking boot or cast for 2 to 4 weeks. If there is no pain or tenderness with walking a stirrup ankle brace, arch support, or lateral heel wedge can help to take tension off of your injured tendons. In most cases, your Doctor will start with non-surgical treatments options. Some of the options your doctor may recommend include drugs or medications like NSAIDs (non-steroidal anti-inflammatory drugs) to manage pain and inflammation. Steroid injections are advised with caution for any type of tendon condition as there is increased risk of tendon rupture. Peroneal Tendonitis Home Conservative Treatment OptionsStep 1 - Reduce Pain and Swelling with Cold CompressionThe first step for conservative treatment of your foot tendonitis is to reduce the swelling to "open up" the area for more blood flow. Anyone in the health-care business knows that your blood supplies the oxygen and much needed nutrients required to heal foot tendonitis injuries. This is why for years, doctors, trainers, and other medical professionals have recommended RICE (Rest, Ice, Compression, Elevation) to treat the pain and swelling of fresh injuries, chronic pain, and after any re-injury. This is important because once blood vessels are blocked or damaged, they can no longer carry oxygenated blood to your damaged tendon and tissues begin to break-down. Without cold compression, tissues break down further because they can't get the oxygen they need to survive. By limiting the amount of damage done to your tendons, you also limit the amount of healing that needs to occur. This is a very important step to heal acute or chronic tendon injuries faster and with less pain! Use a Cold Compress or Ice Pack:
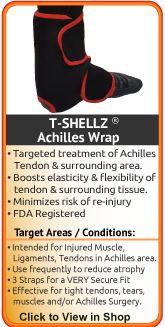
Step 2 - Improve Circulation, Soften Scar Tissue & Prevent Re-Injury with a TShellz Wrap®Once the swelling is gone, moving the tendon and applying a local circulatory stimulation device like the TShellz Wrap® is really what is needed for completing the recovery cycle. This is critical because tendons are known to receive very little natural blood flow and blood flow is really how your body is able to heal itself. When the tendon tissue is damaged, the already-reduced blood flow is decreased down to a trickle which is why movement is encouraged - it helps get blood flow to where it is needed. Blood flow (healthy circulation) is an important part of natural tissue healing. Injured tendons take the nutrients available in local blood flow (like oxygen and healing agents) to get rid of any damaged tissue and start growing healthy tissue. Sometimes Tendons Can't Receive |
         |